T1D Challenges Go Far Beyond Sugar
Living with Type 1 diabetes (T1D) involves managing daily challenges like constant carb counting, blood sugar fluctuations, and "diabetes burnout."
A T1D dietitian or Diabetes Educator can help you navigate these hurdles by creating a personalized plan for T1D meal planning and insulin management, ensuring you maintain energy for school and sports while keeping your levels in range.
Managing Type 1 diabetes is a bit like being a full-time air traffic controller for your own body. While most people’s bodies handle blood sugar automatically, you’re the one in charge of the manual controls. From high school exams to sports practice, the challenges of living with Type 1 diabetes are real, but they don't have to stop you from living your best life.
If you’ve ever felt exhausted after a day of "perfect" numbers, there’s a reason for that. Research shows that people with T1D make nearly 300 health-related decisions every single day. Should you bolus for that extra apple? How will that 3...
T1D Care for Young Children
Managing Type 1 Diabetes in young children requires specialized care because the disease is often more aggressive in toddlers, as their insulin-producing cells are destroyed before they fully mature
Working with a T1D dietitian or Diabetes Educator provides families with proven strategies for carb counting, flexible meal planning, and navigating the unpredictable blood sugar shifts common in early childhood.
A diagnosis of Type 1 Diabetes (T1D) is a life-changing event for any family, but when it affects a toddler or young child, the challenges are uniquely intense. Recent 2025 research has shed new light on why type 1 diabetes (T1D) appears more aggressive in children under the age of seven. Scientists at the University of Exeter discovered that in early-onset cases, the immune system wipes out insulin-producing beta cells before they have a chance to mature. This "aggressive" start means that traditional management often feels like a moving target.
For parents, the burden is immen...
Diabetes-Friendly Meals at Taco Bell
Navigating fast-food menus with diabetes can be tricky, but it's entirely possible to find balanced options
A diabetes dietitian recommends choices with higher protein and fiber to support stable blood sugar. Discover three easy-to-order meals at Taco Bell that are balanced for better blood sugar management.
Facing the fast-food challenge when managing diabetes, whether Type 1 (T1D) or Type 2 (T2D), can feel overwhelming, especially for busy high school students. You need food that's quick, affordable, and won't send your blood sugar on a roller coaster. This is where the guidance of a Type 1 diabetes dietitian or Type 2 diabetes dietitian, often a skilled Diabetes Educator, is invaluable. They teach real-world strategies like carb counting for diabetes and finding quality options on a budget.
A registered dietitian who specializes in diabetes understands that life happens, and sometimes a quick trip through a drive-thru is necessary. The key is making informed choices. A dietiti...
Best A1c Number to Aim for in Diabetes
The A1c is a number that tells you how much sugar (glucose) is stuck onto your red blood cells (glycosylated hemoglobin), giving an average of your blood sugar levels over the past few months
While doctors often aim for an A1c below 7% to reduce the risk of diabetes complications, it is crucial to also monitor your Time-in-Range (TIR) for complete and sustainable blood sugar management tips.
If you have diabetes, what should your A1c be, anyway? And what does A1c even mean?
You hear the term A1c thrown around all the time from the moment you’re diagnosed, whether it's Type 1 diabetes or Type 2 diabetes. You've had this mysterious A1c number thrown in your face at all times, at all opportunities, by your doctors, and you were probably chastised if it wasn't exactly where they wanted it to be for you. It's time to take control of this metric and truly Learn what it means for your health.
Let’s go through the nitty-gritty details on A1c, what it means, and where yours should be for...
Diabetes Dietitian Holiday Guide to Happy Sugars
Discover three essential strategies to keep your blood sugar stable and manage your weight during the holidays
Mastering portion control, nailing medication timing, and carefully watching your drink choices. A T1D dietitian or T2D dietitian can help personalize these tips for sustained blood sugar management.
This time of year is filled with amazing memories, family, and, let's be real, food! But if you're managing diabetes, the holidays can sometimes feel like a blood sugar landmine for both your health and your waistline. The good news? You can enjoy the festivities without the post-holiday regret.
We’ve compiled the ultimate guide, straight from a Diabetes Educator and a diabetes dietitian, to help you master the season. Whether you manage Type 1 diabetes (T1D) or Type 2 diabetes (T2D), these proven secrets will help you keep your blood sugars steady and your stress low.
1. Portion Control is Your Power Move
Think of this as T1D meal planning at its most crucial. The holiday...
Type 2 Diabetes Insulin and Treatment Guide
Type 2 diabetes is not always insulin dependent, but some people may eventually need insulin if their pancreas can’t make enough or if their cells become too insulin-resistant
Treatment for Type 2 diabetes often includes healthy eating, physical activity, blood sugar monitoring, oral medications, and, when needed, insulin therapy. Working with a Diabetes Educator or diabetes dietitian helps individuals build sustainable habits and improve long-term blood sugar control.
Managing diabetes can feel overwhelming, but the right support and information can unlock confidence, control, and hope. Whether you’re newly diagnosed or supporting someone you love, understanding Type 2 diabetes treatment and when insulin becomes necessary is essential. In this guide, you’ll learn what determines insulin use, explore proven blood sugar management strategies, and discover how a diabetes dietitian can make everyday choices feel easier.
Is Type 2 Diabetes Insulin Dependent?
The short answer: sometimes...
Diabetes Dietitian Guide to Stress-Free Travel
For anyone managing diabetes while traveling, preparation is paramount
The ultimate tip for worry-free trips is to pack at least two to three times the amount of diabetes supplies you think you need. This proactive strategy ensures you are fully prepared to maintain excellent blood sugar management, even in the event of unexpected delays, flight cancellations, or extended stays.
The holiday season is here, bringing with it the excitement of travel! But for people living with diabetes, whether that's Type 1 diabetes (T1D) or Type 2 diabetes (T2D), travel can bring unique challenges. Running out of essential supplies is a nightmare no one wants to face.
This is where preparation becomes absolutely KEY. We’re talking about more than just remembering your insulin. We’re talking about the ultimate travel hack that a seasoned diabetes dietitian and Diabetes Educator swears by. This proven tip is essential for happy blood sugars, no matter where your journey takes you.
The Golden Rule ...
Safe Weight Loss for Prediabetes, T1D & T2D

Discover expert weight loss strategies from a diabetes dietitian that safely support blood sugar control for prediabetes, Type 1 diabetes (T1D), and Type 2 diabetes (T2D)
Discover how prediabetes-friendly meal planning, carb counting for diabetes, and simple diabetes-friendly meals can help you lose weight, enhance insulin sensitivity, and feel more energized. Unlock practical tips for sustainable results without sacrificing health.
Losing weight with blood sugar challenges can feel overwhelming, but it’s one of the most effective ways to improve glucose control, boost energy, and reduce long-term health risks. Whether you have prediabetes, Type 1 diabetes (T1D), or Type 2 diabetes (T2D), working with a diabetes dietitian can help you achieve your goals safely and sustainably—and in many cases, help prevent progression to Type 2 diabetes.
Here are proven weight loss tips:
1. Start with Smart Carb Counting for Diabetes & Prediabetes
Carbohydrates directly impact blood sugar. Learn...
Dietitian Strategies for Prediabetes Control

Prediabetes signifies elevated blood sugar and A1C levels, though they remain within a range that offers an opportunity for reversal
Taking a proactive approach is crucial, and collaborating with a diabetes dietitian or educator can significantly improve your blood sugar management. They can help you reduce your A1C and potentially prevent the development of Type 2 diabetes through evidence-based strategies, personalized meal planning principles, and customized exercise routines.
Prediabetes affects over a third of all adults, and the alarming truth is that most are unaware they have it. This situation, while concerning, is also a source of optimism: prediabetes is reversible. With appropriate guidance, many individuals can successfully return their blood sugar levels to a healthy range and prevent the progression to Type 2 diabetes.
This is where a diabetes dietitian, T2D dietitian, or Diabetes Educator becomes a game-changer. Whether you’ve just been told you have prediabetes o...
T1D Challenges Go Far Beyond Sugar
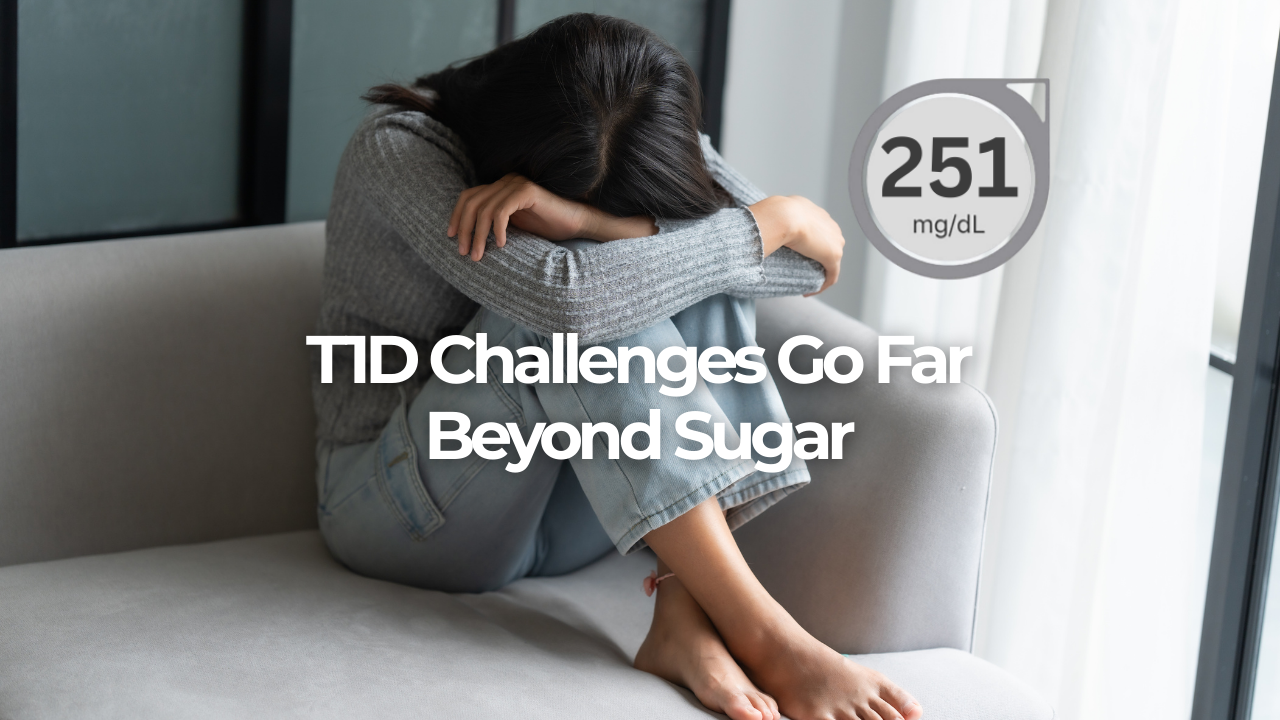
Managing Type 1 diabetes is a bit like being a full-time air traffic controller for your own body.
While most people’s bodies handle blood sugar automatically, you’re the one in charge of the manual controls. From high school exams to sports practice, the challenges of living with Type 1 diabetes are real, but they don't have to stop you from living your best life.
If you’ve ever felt exhausted after a day of "perfect" numbers, there’s a reason for that. Research shows that people with T1D make nearly 300 health-related decisions every single day. Should you bolus for that extra apple? How will that 30-minute gym class affect your levels two hours from now?
This constant mental load can lead to diabetes burnout, a feeling of being completely overwhelmed by the demands of the condition. It’s okay to feel this way, but you don’t have to handle it alone. Working with a Type 1 diabetes dietitian or a Diabetes Educator can help you unlock easier ways to manage these stressors.

